RISK FACTORS AND SYMPTOMS OF AIR POLLUTION ON RESPIRATORY HEALTH
Air pollution has both acute and chronic effects on respiratory health, affecting a number of different systems and organs.
Air pollutants such as nitrogen oxides, ozone, sulphur dioxide, carbon monoxide, and particulate matter affect different parts of the respiratory tract via a variety of mechanisms resulting in respiratory symptoms.
Air quality affects everyone, but some people are more at risk than others. Children and older adults, individuals with pre-existing cardiovascular or respiratory diseases, or genetic polymorphisms are at increased risk of air pollution-related health effects. This can be exacerbated when our body’s defence mechanisms are impaired.
Research is ongoing to identify causal associations of air pollutants with adverse health outcomes, and to uncover plausible biological mechanisms for these effects.
Here, The Clean Breathing Institute discusses the risk factors associated with air pollutants and the respiratory health symptoms associated with air pollution in those individuals who are at increased risk of adverse effects.

How does air pollution affect respiratory health?
Respiratory health effects range from minor upper respiratory irritation to chronic respiratory and heart disease, lung cancer and acute respiratory infections; air pollution can also aggravate pre-existing heart and lung disease.1–6 Short- and long-term exposures have been linked with premature mortality and reduced life expectancy.1
Pollutants with the strongest evidence for adverse effects on respiratory health include particulate matter, ozone, nitrogen dioxide, sulphur dioxide and carbon monoxide. Particulate matter is used as an indicator of air pollution and is usually divided into groups based on particle size.1,3–5 Coarse particulate matter has an aerodynamic diameter of between 10 μm and 2.5 μm, and is referred to as PM10–2.5.6 Fine particulate matter has an aerodynamic diameter of less than 2.5 μm, is referred to as PM2.5 and can penetrate deep into the lung.5,6 (Figure 1).
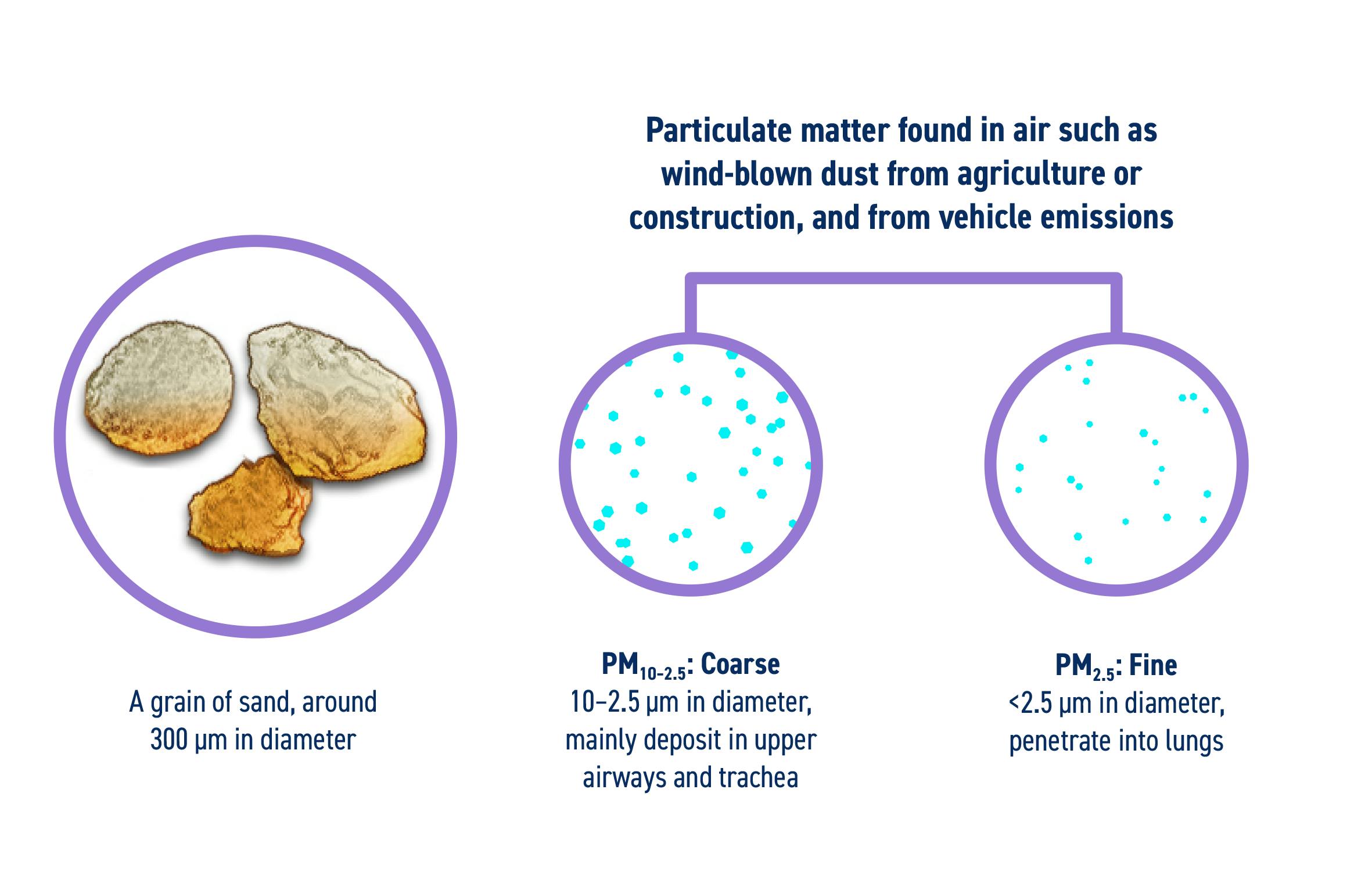
Figure 1. Relative size of particulate matter that can enter the respiratory tract.3,4,6–9 PM, particulate matter. Note PM10-2.5 is represented as 10 μm particles and PM2.5 as 2.5 μm particles shown to scale relative to a grain of silica sand.
Air pollutants including particulate matter of different sizes affect different parts of the respiratory tract resulting in respiratory symptoms and changes in lung function (Figure 2).
The association of fine particulate matter (PM2.5) – which can reach deep into the lungs – with cardiorespiratory disease and mortality is well documented.10 Ultrafine particles (<0.1 μm) can enter the bloodstream and travel to distal organs, and are of considerable concern. No safe level of small particulate pollution has been identified.11
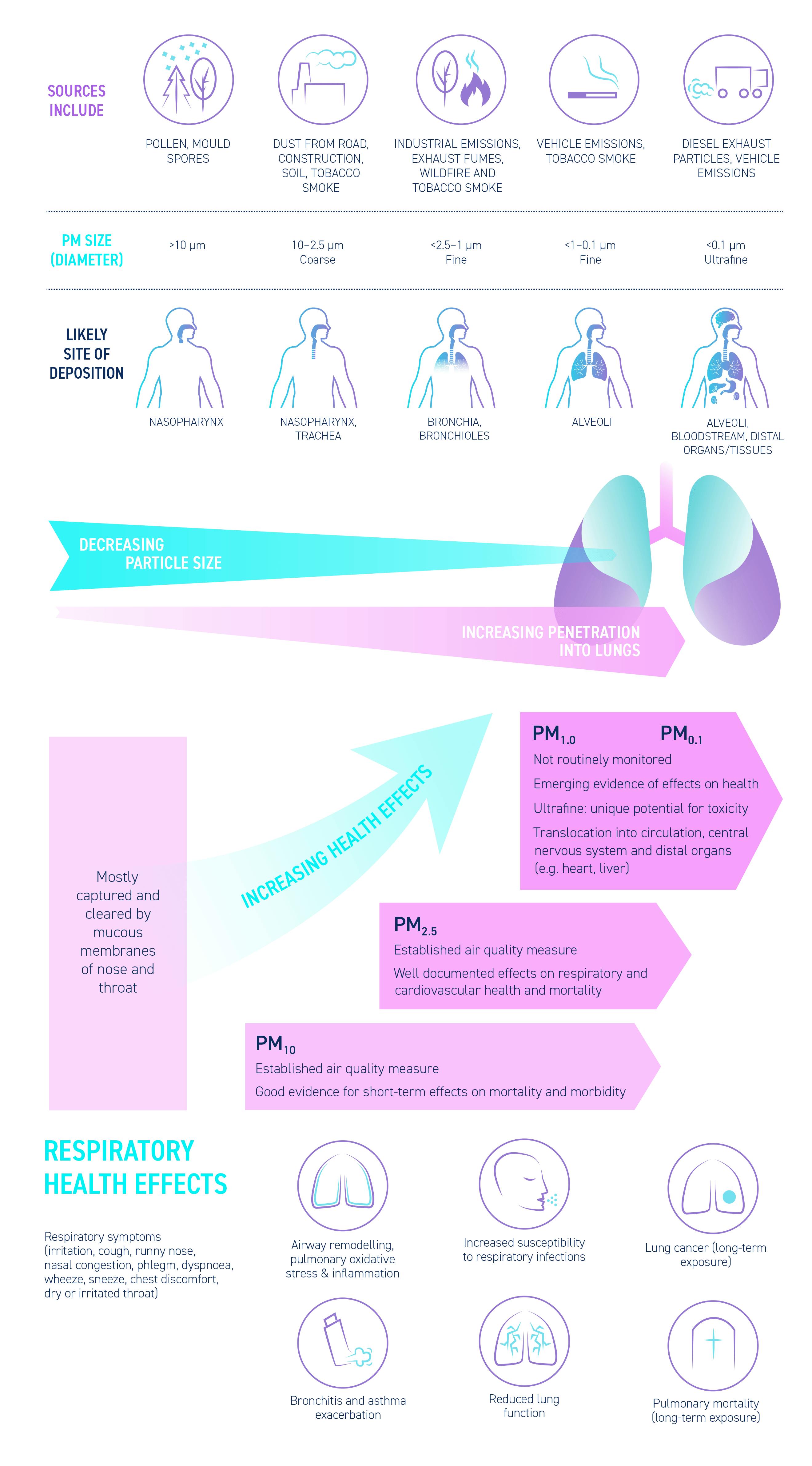
Figure 2. Particulate matter in air pollution, respiratory symptoms and health effects. CNS, central nervous system; PM, particulate matter.1,6–9,12–21
What are the symptoms of air pollution exposure associated with respiratory health?
All types of air pollution, at high concentration, can affect the airways and similar respiratory effects are also observed with long-term exposure to lower pollutant concentrations.1 The most common upper respiratory tract symptoms reported after exposure to air pollution include nose and throat symptoms. These symptoms include non-allergic rhinitis and nasal mucosal erythema, sinusitis, nasal itching, runny nose, nasal congestion, sneezing, dry mouth and throat, productive cough and dry cough, wheezing and dyspnoea.14,15,22,23
Symptoms such as nose and throat irritation, followed by bronchoconstriction and dyspnoea, especially in asthmatic individuals, have been reported after exposure to increased levels of sulphur dioxide24 and nitrogen oxides25. Cough and dry cough, sneezing and runny/stuffed nose have been associated with exposure to PM2.5 and nitrogen dioxide during the first year of life.26,27
Particulate matter that penetrates the lung epithelium can initiate lung inflammation,28 worsening pre-existing lung conditions and exacerbating symptoms of asthma and chronic obstructive pulmonary disease.
Air pollutants such as nitrogen oxides can increase the susceptibility to respiratory infections.29,30 Significant associations have been found between the number of outpatient consultations due to upper respiratory tract infections in Hong Kong and the concentrations of the air pollutants PM10, nitrogen dioxide, ozone, and sulphur dioxide.30
Indoor air pollution and respiratory symptoms
Indoor air pollution in buildings with high levels of airborne particles and gaseous pollutants can lead to complaints of upper respiratory symptoms, such as upper respiratory tract irritation and infection.15,31 These can include nose itching, runny nose, nasal congestion, sneezing, and dry throat, and are linked to indoor carbon dioxide levels and volatile organic compounds.15 Non-allergic rhinitis symptoms have been associated with exposure to particulate matter such as dust, cleaning solvents and strong odours, and are exacerbated by temperature and humidity changes.23
It is important to note that symptoms are not a reliable indicator of whether air pollution is at a level that poses a risk to health. There may be no immediate symptoms, even at relatively high concentrations of exposure.
Prenatal exposure to air pollution
There is mounting evidence for the adverse effects of prenatal air pollution on lung development, respiratory health and development of chronic disease in adulthood.43 Air pollution may also influence pregnancy by inducing systemic inflammation and oxidative stress, and could cross the placenta, and increase maternal susceptibility to infections.44 These effects could impair foetal growth and birth outcomes. BreatheLife – a joint campaign led by the World Health Organization, United Nations Environment, and Climate & Clean Air Coalition – provides tips on reducing prenatal exposure.45

Exposure of children to air pollution
Children are particularly vulnerable to air pollutants because their immune and antioxidant defence mechanisms are still developing and they have a faster breathing rate, taking in more air per unit body weight than adults, resulting in inhalation of higher doses of air pollutants compared with adults. Also, they generally spend more time playing outside, where they may be exposed to pollutants.46
Exposure of healthy individuals to air pollution
Some healthy people are more sensitive to the health effects of air pollution. They may experience health effects at lower air pollution levels than the average person even though they have none of the risk factors noted above. There may be a genetic basis for this increased sensitivity.47,48

How are particles deposited in the respiratory system?
Particle size, water solubility and chemical reactivity all determine where particular air pollutants impact the respiratory tract.14 Highly water-soluble and reactive irritants, such as sulphur dioxide and aldehydes, readily dissolve into the water around the nasal mucosa and initiate an inflammatory response, consequently having greatest impact in the upper respiratory tract.14 Ozone, having medium water solubility, can reach the trachea and bronchi, whereas low solubility gases, such as nitrogen dioxide, are also able to evade the defensive properties of the respiratory tract mucosa and reach the bronchioles and alveoli.14
Particulate matter may be deposited in three different regions of the respiratory system:
- Extrathoracic (nasal, pharyngeal and laryngeal passages)
- Tracheobronchial
- Alveolar (pulmonary)
The key factors affecting deposition include: mode of breathing (mouth, nose or oronasal), breathing pattern (tidal volume, breathing frequency) and particle characteristics (size, shape, mass, hygroscopicity and solubility).8
What are the respiratory tracts defence mechanisms against particulate matter?
The upper respiratory tract comprises the nose, nasal cavity, mouth, throat (pharynx), and voice box (larynx). It plays an important role in monitoring the quality of inspired air as well as air warming and humidifying inspired air,49 and is the first line of defence against air pollutants.14
Different mechanical filters located in the nasopharyngeal (nose hairs and the turbulence in the nasal turbinates), tracheobronchial and alveolar regions protect the airways against inhaled foreign particles.50
The nose acts as the first in a series of protective mechanisms. With its narrow air passages, mucosal folds, and mucous layer covering ciliated epithelial cells, the nose can effectively filter most coarse particles.
Inhaled fine particle pollution deposited on the surface of the airways is cleared by two mechanisms:
- Mucociliary clearance
- Phagocytosis
Mucociliary clearance
Mucociliary clearance is a vital self-clearing process of the airways and removes the vast majority of inhaled particles deposited in the tracheobronchial airways.51,52 On average, 2 litres/day of nasal mucus is produced by the respiratory mucosa to trap particles and moisten airways.53 Mucociliary clearance utilises unique properties of mucus and the specific action of cilia to trap and remove hazardous components of inhaled air, such as some pollutants, bacteria and viruses.22 The cilia beat in a synchronised manner, moving the mucus as well as substances trapped within the mucus, out of the nose so they can be swallowed or expectorated.14,22,54,55
Mucociliary transport in healthy individuals clears most insoluble particles within 24 hours of deposition under normal conditions.56 In chronic conditions such as respiratory diseases like asthma and chronic obstructive pulmonary disease, or in smokers, normal clearance may be impaired and particle retention increases.14,22,54,55
Mucociliary clearance can also be impaired when air pollutants damage the respiratory lining and induce temporary dysfunction of ciliary movement.50 This can result in symptoms such as productive cough and dyspnoea.22 Particles that escape the mucociliary defence mechanisms can enter the lower airways and alveolar region.50
Phagocytosis
Phagocytosis by macrophages is the primary clearance mechanism for removing any foreign material such as particles or microorganisms from the alveolar region.54
Following exposure to particulate matter, alveolar macrophages secrete an array of pro-inflammatory mediators, leading to apoptosis and induction of local and systemic inflammatory responses.57 These macrophages were found to interact with airway epithelial cells to augment the production of a variety of chemokines and cytokines, leading to inflammatory airway responses.58
The efficiency of phagocytosis decreases with decreasing particle size below about 1 μm.59 Ultrafine particles (<0.1 μm) may be deposited in the alveoli and subsequently absorbed into the bloodstream.5,13
Repeated, frequent exposure to particle pollution may overburden the pulmonary defence system.
How do air pollutants exert adverse effects on the respiratory system?
The mechanisms through which air pollutants exert adverse effects include:
- Induction of oxidative stress via the generation of reactive oxygen species, leading to airway inflammation5,60,61
- Influencing immune function, such as the development of allergic disease and response to infections5
- Increasing the risk of upper respiratory tract infections29,30 and symptoms such as rhinitis, sinusitis, sneezing and coughing14,22
Oxidative stress mechanisms and effects on the respiratory health
Combustion-derived particulates can generate free radicals and are highly oxidising.5 Particulate matter and gaseous pollutants appear to induce an inflammatory cytokine response in macrophages via the nuclear factor-κB pathway62 (Figure 3). Exposure to PM2.5 has shown an association with nasal inflammatory cells and cytokine mediators in children,60 while in nasal lavage samples, exposure to ozone combined with heat has been associated with the presence of CC16, which is a marker of nasal epithelial damage.63 Ozone has been associated with persistent structural airway and lung tissue damage.64

Figure 3. Model of oxidative stress mechanisms and effects on the airway. AP-1, activator protein-1; CHO, carbohydrate; DEP, diesel exhaust particles; ecGSHpx, extracellular glutathione peroxidise; ecSOD, extracellular superoxide dismutase; GSH, glutathione; NF-κB, nuclear factor-κB; NO2, nitrogen dioxide; O3, ozone; PM, particulate matter; ROS, reactive oxygen species.65 This material has not been reviewed prior to release; therefore the European Respiratory Society may not be responsible for any errors, omissions or inaccuracies, or for any consequences arising there from, in the content. Reproduced with permission of the © ERS 2018. European Respiratory Journal Jan 2008, 31 (1) 179-197; DOI: 10.1183/09031936.00128106.
Air pollutants influence immune function and affect respiratory health
Diesel exhaust particles (DEPs) can modify the immune response and airway inflammatory processes (Figure 4). Early life exposure to high levels of DEPs in children sensitised to house dust mites by age 4 doubled the risk of developing asthma by age 7 compared with low DEP exposure.66 A systematic review and meta-analysis showed significant associations for black carbon, nitrogen dioxide, PM2.5 and PM10 exposures and risk of asthma development in childhood.67 Air pollutants can also both negatively affect other aeroallergens, such as pollen,68 and enhance allergic response.5,69 Pollen in areas with heavy air pollution expresses greater amounts of allergenic proteins compared with areas with less air pollution.68 Residual oil fly ash has been shown to enhance allergen-induced pulmonary allergic response in mouse models of asthma, suggesting that this type of particulate matter can induce/amplify allergic responses.5 DEPs can act as mucosal adjuvants in enhancing the immunoglobulin E response to allergens and skew cytokine production to a Th2 pattern, amplifying the allergic responses.5 In a randomised and blinded controlled human crossover exposure study, specific allergen-induced proteins in the lung were significantly enhanced with DEP plus allergen compared with either DEP or allergen alone.69

Figure 4 . Mechanistic model of the exposure–disease relationship illustrating a sequential event originating from the exposure to the development of asthma.5 AhR, aryl hydrocarbon receptor; DC, dendritic cell; IgE, immunoglobulin E; iLC, innate lymphoid cells; PAH, polycyclic aromatic hydrocarbon; PM, particulate matter; Th, T helper; VOC, volatile organic compound. Reused/adapted with permission from AME Publishing Company
Air pollutants increase the risk of upper respiratory tract infections
Air pollutants such as nitrogen oxides can increase the susceptibility to respiratory infections.29,30,70 In a study conducted on children in Taiwan, the presence of nitrogen dioxide and ozone peaks lasting for 6 days was significantly associated with increased risk of outpatient visits for acute upper respiratory infections.29
How to manage the health effects of air pollution
Though the respiratory system has remarkable resilience to air pollution via its repeated mobilisation of defence and repair mechanisms, constant exposure to elevated particle pollution will contribute to reduced respiratory function, even in apparently healthy people. Therefore, although exposure to air pollution is difficult to avoid completely, advising patients to take simple steps to reduce exposure may reduce the severity of lung and systemic adverse health effects in both healthy and more sensitive people.
Download our literature review and our advisory meeting summary to find out more about the risk factors associated with air pollution and the effects of air pollution on respiratory health.
RELATED ARTICLES

MANAGEMENT
When avoiding air pollution is difficult, introducing measures to prevent the effects of air pollution and minimise respiratory symptoms can help.
PRACTICAL TIPS & ADVICE

HEALTH BURDEN
Almost every country in the world is affected by air pollution and exposure has been linked with a range of health effects, including increased morbidity and mortality, and respiratory diseases.
IMPACT ON OUR HEALTH



